What Exactly Is GSM ? Genitourinary Syndrome of Menopause
What Exactly Is GSM?
Genitourinary Syndrome of Menopause
If this is your first time hearing the term Genitourinary Syndrome of Menopause (GSM), you’re not alone. GSM is one of the most common—and most misunderstood—medical conditions associated with menopause. It affects the vaginal, vulvar, urethral, and bladder tissues, and it is driven by estrogen deficiency, not by hygiene, sexual activity, or “just getting older.”
This article goes deep into the weeds: the biology, the progression, and the evidence-based treatments—so you understand what’s happening and what can be done about it.
GSM, clearly defined
Genitourinary Syndrome of Menopause (GSM) is a chronic, progressive condition caused by declining estrogen levels that leads to structural and functional changes in the genitourinary tissues.
The term GSM was formally adopted by The North American Menopause Society and International Society for the Study of Women’s Sexual Health to replace outdated terms like vulvovaginal atrophy. Those older labels failed to capture the urinary symptoms, sexual pain, and quality-of-life impact that occur alongside vaginal changes.
GSM can develop during:
-
Perimenopause
-
Natural menopause
-
Surgical menopause
-
Breast cancer treatment involving estrogen suppression
-
Any prolonged hypoestrogenic state
Once established, GSM does not resolve on its own.
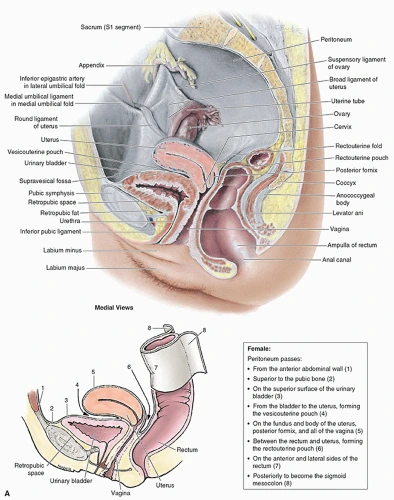
What estrogen actually does in the genitourinary system
Estrogen plays a critical role in maintaining the health of tissues that share a common embryologic origin. In the vagina and lower urinary tract, estrogen:
-
Maintains epithelial thickness and elasticity
-
Supports collagen and smooth muscle integrity
-
Preserves blood flow and nerve sensitivity
-
Keeps vaginal pH acidic, protecting against infection
-
Supports urethral closure pressure and bladder stability
-
Maintains a healthy lactobacillus-dominant microbiome
When estrogen levels fall, these systems deteriorate together.
What’s happening at the tissue level (the “deep weeds”)
Vaginal epithelium changes
-
Thinning of the mucosa
-
Loss of rugae (natural folds)
-
Increased fragility and micro-tearing
-
Reduced lubrication response
Microbiome and pH shift
-
Loss of protective lactobacilli
-
Rise in vaginal pH
-
Increased susceptibility to irritation and infection
Personalized hormone support, weight loss, and aesthetic care for people ready to feel like themselves again.
Urethral and bladder involvement
-
Estrogen receptors in the urethra and bladder trigone lose stimulation
-
Reduced urethral tone
-
Heightened sensory urgency signals
-
Increased frequency of UTIs
This is why GSM symptoms often masquerade as recurrent infections despite negative urine cultures.
Common GSM symptoms
GSM symptoms vary in intensity but commonly include:
-
Vaginal dryness
-
Burning or irritation (vulva or vagina)
-
Itching
-
Loss of natural lubrication
-
Painful intercourse (dyspareunia)
-
Urinary urgency or frequency
-
Dysuria (painful urination)
-
Recurrent urinary tract infections
These symptoms are medical, not cosmetic, and they tend to worsen over time without treatment.
How GSM is diagnosed
GSM is diagnosed clinically, based on:
-
Symptom history
-
Menopausal or hypoestrogenic status
-
Pelvic exam findings when appropriate
A pelvic exam is not mandatory if symptoms and history are clear. Diagnosis does not require hormone testing.
Evidence-based treatment options
1. Local vaginal estrogen (first-line treatment)
Local estrogen therapy is considered the gold standard for GSM by American College of Obstetricians and Gynecologists.
Forms include:
-
Vaginal creams
-
Vaginal tablets
-
Vaginal rings
Benefits:
-
Restores tissue thickness and elasticity
-
Improves lubrication and comfort
-
Normalizes vaginal pH
-
Reduces urinary urgency and UTIs
Local estrogen works by treating the root cause, not just symptoms.
2. Non-hormonal moisturizers and lubricants
These can help with mild symptoms or as adjunct therapy.
-
Moisturizers improve baseline hydration
-
Lubricants reduce friction during intercourse
Limitations:
-
Do not reverse tissue changes
-
Require consistent use
-
Partial symptom relief
3. Vaginal DHEA (prasterone)
-
Converts locally into estrogen and androgens
-
Improves dyspareunia
-
Minimal systemic absorption
Useful for select patients who cannot tolerate estrogen.
4. Oral SERMs (selective estrogen receptor modulators)
-
Act estrogen-like in vaginal tissue
-
Block estrogen in other tissues
-
Systemic medication
Used selectively under medical guidance.
5. Energy-based therapies (laser, radiofrequency)
-
Aim to stimulate collagen remodeling
-
Evidence still evolving
-
Not first-line therapy
-
Often adjunctive
Patients should receive clear counseling on benefits, risks, and alternatives.
What GSM treatment is not
-
Not cosmetic care
-
Not elective or frivolous
-
Not the same as systemic hormone therapy
-
Not something you have to “just live with”
Treating GSM is about function, comfort, urinary health, intimacy, and long-term tissue integrity.
Frequently Asked Questions (FAQs)
1. Is GSM the same as vaginal atrophy?
No. Vaginal atrophy describes tissue thinning only. GSM includes vaginal, vulvar, urinary, and sexual symptoms.
2. Will GSM go away on its own?
No. GSM is progressive without treatment.
3. Can GSM cause recurrent UTIs?
Yes. Estrogen deficiency alters the urinary tract and vaginal microbiome, increasing UTI risk.
4. Is vaginal estrogen safe?
For most patients, yes. Local estrogen has minimal systemic absorption and is widely supported by medical societies.
5. Do lubricants fix GSM?
They help symptoms but do not reverse tissue changes.
6. Can GSM affect libido?
Indirectly, yes. Pain and irritation can suppress desire and arousal.
7. Does GSM only affect sexually active women?
No. Symptoms occur regardless of sexual activity.
8. Can breast cancer survivors have GSM?
Yes, and it is common. Treatment options should be individualized with oncology-informed care.
9. Is painful urination always a UTI?
No. Dysuria is a common GSM symptom even with negative cultures.
10. When should treatment start?
As soon as symptoms appear. Early treatment prevents progression.